You Can Get STIs From Kissing—Here's Which Ones and How To Avoid Them
Did You Know Menopause Can Impact Oral Health? Most Brits Have No Idea
A woman feeling pain, holding her cheek with hand, suffering from bad tooth ache.
gettyMenopause affects women's bodies in many ways, and awareness that it's more than hot flashes and night sweats is growing.
But plenty of us still don't realize just how wide-ranging the impacts of the change of life can be, reinforcing negative stereotypes and leaving women unprepared.
Some 90% of Brits don't know there's a link between menopause and oral health, according to the results of a survey commissioned by independent U.K. Health provider Bupa.
Of 2,001 people quizzed for the research, 86% of women and 94% of men didn't know that changes to their teeth, tongue or gums can be linked to menopause.
In reality, it can lead to gum disease, toothache and even tooth loss. But with the right care and treatment, many oral health issues can be resolved.
Why does menopause affect oral health?Hormone levels fluctuate as a woman approaches menopause. Estrogen drops and eventually a woman's periods will stop altogether.
We may think of estrogen as a sex hormone, but it actually plays a key role in all kinds of physiological processes.
"We need estrogen for pretty much every single bodily function that a woman has," Dr Sam Wild, family doctor and clinical lead for womens' health at Bupa, told me. "We need it for our healthy teeth, for our bones, for our ligaments, for the membranes inside our mouth as well. So as the levels fall, it makes women more susceptible to oral health problems."
It can also change the appearance of the mouth, according to dentist Jason B Cellars, who runs Seacliff Dental in California. He told me that reduced blood supply to the gums increases the risk of recession, which can make teeth appear longer and darker.
"The other concern is bone loss from periodontal disease," he added. "With less defence against infection and disease, bone loss around teeth can lead to cavities."
Dry mouthDry mouth is one of the most common oral health problems women face during menopause.
Menopause is linked both to a drop in the production of saliva and a change in its composition, Bupa Dental Care hygienist and head of hygiene and therapy Caitlin Miller told me.
"Saliva can become quite sticky and thick," she said. "That causes problems with speech, swallowing, and it can lead to bad breath."
That's because having a dryer mouth makes it easier for bacteria to grow. This can lead to tooth decay, gum disease, toothache, sensitivity and ultimately tooth loss.
"Our saliva is what neutralizes our mouths when we eat and it plays a huge role in preventing cavities," Dr Cellars said. When salivation goes down, the chances of developing cavities "goes up drastically," he added.
Burning mouthAnother common problem linked to menopause is known as "burning mouth."
"This is just a constant pain that can be felt anywhere in the mouth and the throat," said Dr Wild. "It can be really, really debilitating and it can alter people's taste as well, particularly to salty foods and sour foods."
A woman attends a dentist appointment. Regular dental check-ups are more important than ever during ... [+] menopause.
getty Mental healthA lot of women suffer with mental health issues during menopause and perimenopause, and oral health issues can make this worse.
Women can "lose their self-confidence and their self-esteem because of all these changes that are going on physically and mentally," said Dr Wild. "Feeling that you've got bad breath on top of that is really not good."
Mental health is related to oral health beyond the latter's impact on self esteem.
Researchers are investigating how bacteria in the mouth might affect other parts of the body.
Improving the health of your mouth, Miller told me, may alter the composition of bacteria in other parts of your body.
"If we're sorting out bacteria in the mouth, which is the portal to the rest of the body, we're helping gut health," she said. And as a growing body of research suggests, the bacteria in your belly may influence the health of your brain and your mental wellbeing.
Maintaining oral health during menopauseMany women don't know about the impact of menopause on their oral health. They might not realise they can get help from their dentists or hygienist, or that they might need to take more care of their teeth than they used to.
Lots of oral health problems can be improved and even resolved with good oral hygiene. That means brushing your teeth twice a day with fluoride toothpaste and regularly cleaning between your teeth with interdental brushes or floss.
Visiting a dentist or hygienist regularly can help you spot emerging issues as soon as possible. They may recommend products like sprays to help ease dry mouth.
They can also show you how to correctly brush and floss your teeth — something often taught in childhood and never revisited.
"I gave a talk recently to a room of 80-year-olds," said Miller. "I had a woman come up to me and say, 'I never knew I should have done it like that.'"
Lifestyle changes like cutting down on alcohol, stopping smoking, eating a healthy diet and getting enough sleep can also help improve mouth health.
Many women going through menopause drink more alcohol to help cope with the symptoms. But in reality, this can make menopause symptoms — including oral health issues — worse.
"It's really the advice we would give to anybody to a certain degree," said Dr Wild. "All this normal advice becomes even more important during menopause."
Medical treatmentLifestyle, she added "is imperative." But it isn't always enough to manage symptoms.
Doctors may ultimately prescribe hormone replacement therapy to help ease the symptoms of menopause and perimenopause — and women may be eligible before they realize.
"I think a lot of women feel that they can't have HRT until their periods have stopped, and that's not true," Dr Wild said.
Reach out to your doctor to get more information about HRT, she added. "Make that informed decitions as to whether treatment is right for you."
Unspoken Symptoms: Exploring The Oral Manifestations Of Rheumatic Diseases
Rheumatic diseases include a range of disorders commonly marked by joint pain and inflammation. While these conditions often have systemic effects, oral symptoms — such as swollen gums, jaw pain, and dry mouth — frequently emerge before more pronounced joint or systemic manifestations. Although these oral symptoms may be subtle and easily overlooked, they can be crucial early indicators of the underlying disease.
Understanding the potential associations between inflammatory diseases and oral health allows for a more comprehensive approach to diagnosing rheumatic diseases. Early identification can lead to timely rheumatologist referral, possibly enhancing patient outcomes.1 The following sections describe and define rheumatic diseases that exhibit early evidence of disease progression through orofacial signs and symptoms.
Oral Manifestations, Clinical Presentations, and Diagnosis Rheumatoid Arthritis and Periodontal DiseaseResearch suggests that rheumatoid arthritis (RA) may heighten the risk for periodontal disease. In 2016, Konig et al identified the bacterium Aggregatibacter actinomycetemcomitans as a potential trigger of chronic gum inflammation, leading to periodontal disease. This bacterium produces altered proteins that the immune system misidentifies as threats, potentially exacerbating RA symptoms. While there is strong evidence linking oral flora to RA, it should be noted that not all patients with periodontal disease develop RA.2
Periodontal disease is characterized by symptoms such as bleeding and tender gums, receding gums, deepening pockets around the teeth, and eventual tooth mobility. Nonsurgical interventions such as laser therapy and deep cleaning beneath the gumline are used to address and slow disease progression.3 Research suggests that treating periodontal disease might improve RA activity, decrease erythrocyte sedimentation rate and C-reactive protein levels, and reduce tumor necrosis factor levels.4
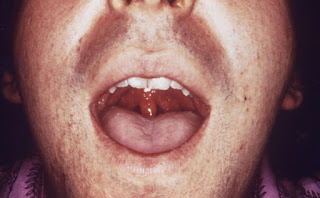
Systemic Sclerosis and Restricted Mouth OpeningSystemic sclerosis (SSc), or scleroderma, is a chronic autoimmune disorder marked by skin and connective tissue thickening. The causes and mechanisms of fibrosis and sclerosis are not fully understood. The condition often affects oral and facial tissues, starting with tongue rigidity and facial skin hardening leading to a mask-like appearance, thin white lips, a sharp nose, and deep wrinkles.5
According to research conducted by Paquette and Falanga, survey results from patients with SSc revealed that circumoral wrinkles (80%), a tighter mouth (77%), thin lips (73%), and loss of facial lines (68%) were the most pronounced aesthetic concerns, occurring more frequently than other nonfacial SSc symptoms.6
The primary oral manifestation of SSc is microstomia, or reduced mouth opening, caused by sclerosis of the perioral soft tissues. This condition can impact mastication, mandibular movement, and oral hygiene, leading to an increased incidence of oral diseases such as caries and periodontal conditions. Mouth stretching exercises are generally the most effective treatment for microstomia, with splint therapy as an option in severe cases.7
Systemic Lupus Erythematosus and Oral LesionsOral lesions associated with active systemic lupus erythematosus (SLE) often present as red ulcers with a white halo and white radiating lines referred to as discoid lesions. These lesions, which may be painful or painless, are usually found inside the cheeks, on the hard palate, or on the lower lip. It is vital that patients inform their physician as soon as these lesions are observed, as biopsy remains the most reliable method to confirm whether oral lesions are related to SLE.8
Oral lesions may respond to topical or intralesional steroids, but antimalarial drugs might be needed for resistant cases. Managing active systemic disease generally helps control oral lesions.9
Future DirectionsWhile rheumatic diseases are often associated with inflammation, oral symptoms may arise before other aligning symptoms. Oral manifestations are key diagnostic clues for rheumatic diseases, which is why collaboration between rheumatologists and dental practitioners is crucial for early diagnosis.
A multidisciplinary approach may be beneficial for managing symptoms and preventing complications. For example, patients with RA may have difficulties with oral hygiene due to joint pain or stiffness, so tailored oral care recommendations and assistance with oral hygiene techniques can be useful.10 Ensuring a comprehensive evaluation during routine dental check-ups, such as incorporating questions about systemic health and medication use into patient interviews, can also help identify underlying rheumatic diseases.


Comments
Post a Comment